Hormones for Cancer Survivors: Optimizing Your Health After Treatment
[videopress kNjyZnUp]
If You Feel Like Cancer Treatment Stole More Than Just Your Tumor
You beat cancer. The scans are clear. Your oncologist shook your hand and said “see you in six months.” Everyone celebrated your survival. Your friends tell you how lucky you are.
But here’s what nobody wants to talk about: you feel worse now than you did during treatment.
The Hidden Aftermath of Cancer Survival
You’re exhausted in a way that has nothing to do with how much you sleep. Your sex drive didn’t just diminish—it vanished completely. You’ve gained weight despite eating less. Your brain feels wrapped in fog. You can’t build muscle no matter how hard you train. You wake up multiple times every night. Your moods swing wildly. You look in the mirror and don’t recognize the person staring back.
The Dismissive Responses You Keep Hearing
And when you mention any of this to your doctors, they give you the same dismissive responses over and over:
“That’s just part of getting older.” “You should be grateful you survived cancer.” “These symptoms are normal after chemotherapy.” “Give it more time—it’ll get better.” “There’s nothing we can do about that.”
A Specialist’s Perspective on Hormonal Devastation
Let me tell you something after thirty years treating cancer patients and now specializing in survivorship: these responses are not just inadequate. They’re a tragedy. They represent one of the greatest failures in modern oncology—a failure I witnessed firsthand for decades before I finally found a better way.
I’m Dr. Ramesh Kumar, board-certified medical oncologist and Harvard-trained integrative medicine physician. I built six cancer centers across Florida’s Treasure Coast. I’ve treated over ten thousand cancer patients. And for years, I watched my patients suffer from hormonal devastation that chemotherapy and radiation caused—devastation that nobody acknowledged, nobody treated, and nobody even discussed.
The truth is this: chemotherapy and radiation therapy don’t just kill cancer cells. They systematically destroy hormone-producing organs throughout your body. Your thyroid. Your adrenal glands. Your ovaries or testicles. Your pituitary gland. These treatments create hormonal chaos that conventional medicine simply abandons you to live with.
But it doesn’t have to be this way.
Educational Disclaimer: This article provides educational information only and does not constitute medical advice for your specific situation. Hormone optimization in cancer survivors requires individualized medical assessment and monitoring. Always consult with qualified healthcare professionals—ideally those with both oncology and hormone optimization expertise—before beginning any hormone therapy. The information presented here is based on current medical evidence and clinical experience but may not be appropriate for all patients.
The Tragedy Nobody Talks About: How Cancer Treatment Destroys Your Hormones
Let me explain what’s actually happening inside your body after chemotherapy and radiation. This is the conversation your oncologist should have had with you before you started treatment, but probably didn’t.
How Cancer Treatments Damage Hormone-Producing Organs
Cancer treatments work by attacking rapidly dividing cells. That’s why they kill cancer. But they also attack other rapidly dividing cells in your body—including the cells in your hormone-producing organs. The medical term for this is chemotherapy-induced gonadal toxicity, radiation-induced hypothyroidism, treatment-related hypogonadism. Premenopausal women are particularly at risk for ovarian damage from these treatments, which can lead to estrogen deficiency and premature menopause. But what these clinical terms really mean is this: your body’s hormone factories got bombed alongside your cancer, often resulting in estrogen deficiency, especially in women.
Hormonal Damage in Men: Testosterone Loss

For men, chemotherapy damages Leydig cells in the testicles—the cells that produce testosterone. Certain chemotherapy agents like cyclophosphamide, cisplatin, and MOPP regimens are particularly notorious for this. Radiation to the pelvis, brain, or whole-body radiation for bone marrow transplant can devastate testosterone production. The result is what we call post-chemotherapy hypogonadism—testosterone levels that plummet to castrate levels and may never fully recover.
Hormonal Damage in Women: Premature Menopause and Ovarian Insufficiency
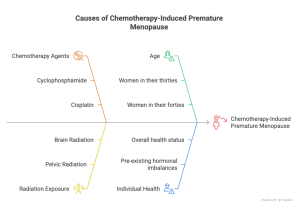
Chemotherapy-Induced Premature Menopause and Ovarian Insufficiency
For women, the damage is often even more dramatic. Chemotherapy can trigger premature menopause, sometimes called chemotherapy-induced menopause or chemotherapy-induced ovarian insufficiency. Women in their thirties and forties suddenly experience hot flashes, night sweats, vaginal dryness, complete loss of libido, mood instability, and bone density loss—all because their ovaries stopped functioning.
These are classic menopause symptoms, with hot flashes and night sweats being key vasomotor symptoms that significantly impact quality of life. Unlike natural menopause that occurs gradually over years, chemotherapy-induced menopause happens suddenly and severely.
Hormone Preservation and Replacement in Ovarian Cancer Subtypes
Certain ovarian cancer subtypes, such as germ cell tumours, require different management considerations for hormone preservation and replacement. Oncologic treatments can induce premature ovarian insufficiency, leading to these menopausal symptoms in cancer survivors, and these issues are particularly relevant in the context of ovarian cancer.
Menopausal Hormone Therapy for Symptom Management in Cancer Survivors
After describing the symptoms of premature menopause, clinicians may consider menopausal hormone therapy for symptom management, with special considerations in cancer survivors.
Radiation-Induced Thyroid Damage and Hypothyroidism
But testosterone and estrogen are just the beginning. Radiation to the neck—common in head and neck cancers, Hodgkin’s lymphoma, and thyroid cancer—frequently damages the thyroid gland, causing hypothyroidism. Your metabolism crashes, and you develop profound fatigue, weight gain, cold intolerance, depression, brain fog, and hair loss. This can develop months or even years after radiation treatment ends.
Damage to the Hypothalamic-Pituitary-Adrenal Axis
Chemotherapy also damages the hypothalamic-pituitary-adrenal axis, which is the communication system between your brain and adrenal glands. This creates a condition similar to adrenal insufficiency where your body can’t produce adequate cortisol in response to stress. You feel chronically fatigued, can’t handle stress, experience low blood pressure and dizziness, and have a diminished sense of wellbeing.
Growth Hormone Deficiency After Cancer Treatment
Growth hormone production from the pituitary gland often declines after cranial radiation or certain chemotherapy regimens. This leads to decreased muscle mass, increased body fat (especially visceral fat around your organs), reduced bone density, fatigue, and impaired quality of life.
The Impact of Hormone-Sensitive Tissues and Estrogen Receptor Status
Damage to hormone-sensitive tissues, such as breast tissue, and the role of estrogen receptor status are important considerations in understanding the risks and management of hormone therapies after cancer. Progesterone receptor status also influences tumor growth, prognosis, and decisions regarding hormone therapy safety. These factors influence both the safety and effectiveness of treatment, especially in breast cancer survivors.
The Irony of Untreated Hormonal Devastation Mimicking Cancer Recurrence
And here’s the cruel irony: all of these hormonal problems create symptoms that are identical to what cancer patients fear most—cancer recurrence. Fatigue, weight changes, cognitive difficulties, pain, mood disturbances. Patients come to me terrified that their cancer is back, when what they’re actually experiencing is untreated hormonal devastation from the treatment that saved their life.
The Medical Community’s Silence on Hormonal Damage
The worst part? Most oncologists know this happens. They just don’t do anything about it. They focus exclusively on tumor control—on five-year survival rates, progression-free survival, overall survival. They celebrate when the scans are clear. But they completely ignore the fact that they’ve left their patients with a quality of life that makes them wish they’d never survived at all.
I know this because I did it myself for twenty years. I gave patients chemotherapy knowing it would destroy their hormone production. I delivered radiation knowing it would damage their thyroid. And then I shook their hand, told them they were cured, and sent them on their way to suffer in silence.
That’s the tragedy. And it’s inexcusable.
Why Your Doctors Won’t Help You (And Why I Finally Can)
The Gap in Hormone Care After Cancer Treatment
After I completed my Harvard Medical School training in integrative medicine in 2016, I began to understand why this massive gap in cancer care exists. The reasons are complex, but they all come down to the same fundamental problem: conventional medicine has created a system where nobody takes responsibility for your hormones after cancer treatment.
Limitations of Oncologists, Primary Care, and Endocrinologists
Your oncologist doesn’t feel qualified to manage hormones. They treat cancer, not optimize testosterone, estrogen, thyroid, or cortisol. Most have never prescribed bioidentical hormone replacement therapy. They fear liability. They worry that replacing hormones might increase cancer recurrence risk—even when the evidence doesn’t support that fear for many cancer types. So they avoid the topic entirely.
Your primary care physician is even more hesitant. They see “history of cancer” in your chart and become paralyzed with fear. They don’t want to do anything that might be perceived as risky. They don’t understand the nuances of which hormones are safe for which cancer types.
They certainly don’t know how to navigate controversial questions like testosterone replacement in prostate cancer survivors or estrogen therapy in breast cancer survivors. So they tell you “that’s above my pay grade” and refer you back to your oncologist—who already told you they can’t help.
Your endocrinologist might replace your thyroid hormone if your levels are severely low, but they rarely optimize it. They aim for “within normal range” rather than “optimal for your age and symptoms.” They almost never address sex hormones, growth hormone, or comprehensive hormone optimization. And they definitely don’t understand the unique considerations in cancer survivors.
Risks of Non-Specialized Hormone Clinics
Meanwhile, anti-aging clinics and testosterone replacement therapy clinics have popped up everywhere promising to restore your vitality. But here’s the problem: most of these clinics are run by nurse practitioners or physician assistants following cookie-cutter protocols. They take your blood, see that your testosterone is low, and prescribe you testosterone—period. They don’t ask detailed questions about your cancer history. They don’t understand the difference between hormone-sensitive and non-hormone-sensitive cancers. They don’t know how to monitor for recurrence. They don’t collaborate with oncologists. They’re essentially treating you like any healthy person walking in off the street.
This is dangerous.
Examples of Unsafe Practices
I’ve seen men with prostate cancer histories prescribed high-dose testosterone by clinics that never even asked about their Gleason scores. I’ve seen breast cancer survivors given compounded bioidentical estrogen by naturopaths who had no understanding of hormone receptor status.
I’ve seen patients started on growth hormone peptides, thyroid medications, and DHEA in combinations that were never medically indicated and never properly monitored. It is also critical to understand drug interactions with tamoxifen treatment, especially when hormone or antidepressant therapies are involved, as these can impact the effectiveness and safety of care.
The Dangers of Online Telehealth Hormone Services
The internet has made this even worse. Telehealth services now let you fill out an online questionnaire, do a blood test at a local lab, and get testosterone or thyroid medications shipped to your door—all without ever speaking to a physician who reviewed your actual medical records. These services explicitly market to cancer survivors by claiming they’re “patient-friendly” compared to conventional doctors who “refuse to help.”
Warning Signs to Watch For
Let me be absolutely clear: if a provider prescribes you hormones without reviewing your actual cancer pathology reports, without understanding your specific treatments, without checking current tumor markers or surveillance imaging, and without coordinating with your oncologist—run. That provider is either incompetent or profit-driven, and either way, they’re putting you at risk.
Here are specific red flags that should make you walk out immediately:
They guarantee results.
- Any clinic promising to “restore you to your twenties” or guarantee specific outcomes is lying. Hormone optimization is complex, individualized, and requires careful titration and monitoring. Legitimate physicians never guarantee results.
They don’t ask detailed cancer questions.
- If they’re not asking about your cancer type, stage, grade, specific treatments, dates of treatment, current surveillance schedule, and recent imaging results—they don’t understand oncology and shouldn’t be treating cancer survivors.
They use a one-size-fits-all protocol.
- If they put every man on the same testosterone dose, every woman on the same estrogen/progesterone ratio, or every thyroid patient on the same medication without individualizing—they’re practicing cookbook medicine, not personalized medicine.
They don’t monitor appropriately.
- Hormone replacement requires regular blood work, symptom monitoring, and in cancer survivors, coordination with oncology surveillance. If they don’t check hormone levels, tumor markers, and other safety parameters every three to six months—they’re being negligent.
They dismiss your oncologist’s concerns.
- If your oncologist is hesitant about hormone replacement and the hormone clinic tells you “your oncologist just doesn’t understand modern hormone therapy”—be very cautious. Sometimes oncologists are overly conservative, but sometimes they identify legitimate risks that the hormone clinic ignores.
They push peptides and experimental therapies aggressively.
- Peptide therapy, growth hormone secretagogues, and various “cutting-edge” anti-aging interventions are being marketed heavily right now. Some have legitimate uses. Many are untested in cancer survivors. If a clinic is more excited about selling you BPC-157, thymosin beta-4, or CJC-1295 than about understanding your cancer history—they’re more interested in profit than in your safety.
They never say no.
- A legitimate physician should sometimes tell you that a particular hormone isn’t appropriate for your situation. If every patient gets every hormone they request regardless of cancer type—that’s a sales operation, not a medical practice.
The Safe Path: Integrative Oncology Expertise
The safest approach is to work with a physician who has both oncology expertise and hormone optimization training. This is rare, which is exactly why we created the Restore pathway at LifeWell MD. You need someone who understands both worlds—who knows when hormones are safe, when they’re risky, when they require additional consultation, and when they’re simply inappropriate regardless of how much you want them.
You also need a physician who will have honest conversations about uncertainty. The truth is that for some clinical scenarios, we don’t have perfect data. We have emerging evidence, expert opinions, theoretical concerns, and risk-benefit calculations—but not randomized controlled trials that definitively answer every question.
Authoritative sources such as CA Cancer J Clin provide valuable cancer statistics and evidence-based guidelines, but even these resources acknowledge areas where uncertainty remains. A good physician will acknowledge this uncertainty, discuss it openly, and help you make informed decisions rather than pretending they have all the answers.
Three Essential Questions Before Starting Hormone Therapy After Cancer
Before you commit to any hormone optimization program as a cancer survivor, you need to ask three critical questions. The answers will immediately tell you whether you’re dealing with a knowledgeable, safety-conscious physician or someone who shouldn’t be treating cancer survivors.
Additionally, ask about non-hormonal alternatives such as selective estrogen receptor modulators (SERMs), which can help manage menopausal and vaginal symptoms or support bone health in certain cancer survivors without stimulating breast tissue.
Question 1: What specific aspect of my cancer history affects which hormones are safe for me?
Listen carefully to how they answer this. A knowledgeable physician should be able to explain the specific characteristics of your cancer that influence hormone safety decisions.
The right answer sounds like this: “You had stage II ER-positive, PR-positive, HER2-negative invasive ductal carcinoma treated with lumpectomy, chemotherapy, and five years of tamoxifen which you completed two years ago. Because your tumor was hormone receptor-positive, we need to be very cautious with estrogen replacement.
However, we can safely optimize your thyroid function, address your vitamin D deficiency, and consider DHEA supplementation. If your vaginal atrophy is severe, we can discuss ultra-low-dose local vaginal estrogen which doesn’t significantly increase systemic levels.”
Or: “You had stage III colon cancer treated with surgery and FOLFOX chemotherapy. Colon cancer is not a hormone-sensitive malignancy, so we have much more flexibility with hormone optimization. Your chemotherapy likely damaged your Leydig cells, which explains your low testosterone. We can safely replace your testosterone, optimize your thyroid, and address any other hormonal imbalances without increasing your colon cancer recurrence risk.”
Warning signs that should make you leave:
- They can’t tell you whether your cancer was hormone-sensitive or not
- They don’t ask to see your pathology reports
- They say “all cancers are in the past, so hormones are fine now”
- They give vague answers like “we’ll just start with low doses and see how you feel”
- They seem unfamiliar with terms like ER/PR status, Gleason score, or hormone-receptor positive
If they can’t explain the specific biology of your cancer and how it affects hormone safety decisions, they don’t understand oncology well enough to be treating you.
Question 2: How will you monitor me for both hormone optimization and cancer surveillance?
This question reveals whether the provider understands that cancer survivors need more comprehensive monitoring than the general population.
The right answer includes:
- Regular hormone level testing (typically every 3-6 months initially, then every 6-12 months once stable)
- Coordination with your oncology surveillance schedule
- Monitoring of tumor markers if you have a cancer type with reliable markers (PSA for prostate cancer, CEA for colorectal cancer, etc.)
- Understanding of your imaging schedule and willingness to review results
- Symptom monitoring for both hormone optimization and potential recurrence
- Adjustment of therapy based on both hormone levels and clinical response
They should be able to say something like: “We’ll check your testosterone, estradiol, thyroid function, and other relevant hormones every three months initially. I’ll want to see your latest PSA results and coordinate with your urologist’s surveillance schedule. If you develop any concerning symptoms—bone pain, unexpected weight loss, new masses—we’ll have a low threshold for additional imaging. I’ll be in communication with your oncologist about your treatment plan.”
Warning signs:
- They only check hormones, never tumor markers
- They don’t ask about your oncology surveillance schedule
- They’ve never coordinated care with an oncologist
- They say “your cancer is cured, so we don’t need to worry about that”
- They have no plan for what to do if you develop concerning symptoms
Appropriate monitoring requires understanding both hormone optimization and cancer surveillance. If they only understand one, they’re not qualified to treat cancer survivors.
Question 3: Under what circumstances would you NOT treat me with hormones, or what would make you stop treatment?
This is perhaps the most important question because it reveals whether the provider has appropriate medical judgment or is just trying to sell you hormones.
A good answer includes specific scenarios where they would decline treatment or discontinue therapy:
- “If your cancer recurs or progresses, we would immediately stop hormone therapy and reassess”
- “If you develop significantly elevated PSA or other tumor markers, we’d pause treatment pending oncology evaluation”
- “If you’re within six months of completing chemotherapy, I’d prefer to wait until your system has had more time to recover”
- “If your cancer was high-grade, high-stage, or you had recent treatment, I might want to consult with a hormone specialist like Dr. Morgentaler before proceeding”
- “If you’re not tolerating the therapy well or not getting benefits that justify potential risks, we’d discontinue”
A physician who is appropriately cautious should be able to articulate clear situations where they would say no or stop treatment. This demonstrates clinical judgment and prioritization of your safety over revenue.
Major red flags:
- They can’t think of any scenario where they wouldn’t treat you
- They say “we can treat everyone safely”
- They minimize risks or dismiss concerns
- They act offended that you’re questioning their judgment
- They pressure you to start immediately without adequate evaluation
Remember: a good physician should sometimes tell you no. If every patient gets every hormone they want regardless of individual circumstances, you’re dealing with a sales operation disguised as a medical practice.
What Real Restoration Looks Like: The LifeWell MD Restore Pathway
Remarkable Transformations Through Proper Hormone Optimization
When physicians do hormone optimization correctly—with proper oncology oversight, individualized protocols, comprehensive monitoring, and genuine concern for your wellbeing—the transformation can be remarkable.
I’ve seen men in their fifties who could barely get through a workday regain the energy and vitality they had in their thirties. I’ve watched their muscle mass return, their abdominal fat shrink, their brain fog clear, their mood stabilize, and their confidence return.
I’ve seen women who thought they’d never feel sexual desire again rediscover intimacy with their partners. I’ve watched them stop waking up drenched in sweat multiple times a night. I’ve seen their anxiety diminish, their weight normalize, their cognitive function improve, and their sense of being fully alive return.
Comprehensive Survivorship Care Beyond Hormone Optimization
But here’s what’s important to understand: hormone optimization is just one component of comprehensive cancer survivorship care. At LifeWell MD, our Restore pathway addresses the full spectrum of what conventional oncology leaves behind. As part of comprehensive care, we also monitor for long-term risks such as cardiovascular disease in cancer survivors receiving hormone therapy.
We optimize your metabolic health because chemotherapy often creates insulin resistance, mitochondrial dysfunction, and metabolic syndrome. We support your detoxification pathways because chemotherapy metabolites and medication burden often overwhelm your liver.
We address nutritional deficiencies because cancer and its treatments deplete vitamins, minerals, and micronutrients essential for healing. We use evidence-based therapies like our NovoTHOR Red Light Therapy bed to support mitochondrial function and tissue healing through photobiomodulation.
Individualized Hormone Therapy Based on Cancer History
When appropriate—and only when appropriate for your specific cancer history—we incorporate hormone optimization. For some patients, this means comprehensive replacement of testosterone or estrogen. For others, it means optimizing thyroid function and supporting adrenal health while avoiding sex hormones. For others still, it means detailed consultation, collaboration with specialists, and careful consideration before deciding whether hormone therapy makes sense.
The point is this: we make decisions based on your individual cancer biology, your specific treatments, your current health status, your quality of life impairment, and your personal values and risk tolerance. Not based on protocols, not based on what we can bill, and certainly not based on ignoring your cancer history and treating you like everyone else.
Physician-Led, Oncology-Informed Integrative Medicine
This is physician-led, oncology-informed, evidence-based integrative medicine. Clinical oncology plays a crucial role in developing survivorship care plans that address the unique needs of each patient. Ongoing breast cancer research continues to inform and improve survivorship outcomes, guiding our evolving approach to care.
This is what happens when you combine board certification in medical oncology with membership in the Androgen Society and International Society for Sexual Medicine. This is what’s been missing from cancer care—and it’s what we offer at LifeWell MD.
You Have Every Right to Feel Alive
Challenging Common Misconceptions About Post-Cancer Symptoms
Let me return to where we started: the dismissive responses you’ve been getting when you mention your symptoms.
“That’s just part of getting older.” No, it’s not. Treatment-induced endocrine damage causes hormone deficiency at forty or fifty or sixty—not normal aging.
“You should be grateful you survived cancer.” Gratitude and quality of life are not mutually exclusive. You can be grateful for survival and still deserve to feel good.
“These symptoms are normal after chemotherapy.” Common, yes. Normal, no. And more importantly—treatable.
“Give it more time—it’ll get better.” For many hormonal problems, time alone won’t fix anything. Your testicles won’t spontaneously recover from chemotherapy damage. Your thyroid won’t heal itself after radiation.
“There’s nothing we can do about that.” This is simply false. We can do a great deal—safely, effectively, and with appropriate monitoring.
You Deserve More Than Survival
You survived cancer. That’s an incredible accomplishment. But survival is not enough. You deserve vitality. You deserve energy, mental clarity, healthy body composition, stable mood, quality sleep, and yes—sexual function and intimacy. You deserve to recognize yourself in the mirror. You deserve to feel like yourself again.
You do not have to accept profound fatigue, weight gain, brain fog, depression, and loss of vitality as the price of surviving cancer. These symptoms are not your fault, they’re not all in your head, and they’re not something you just have to live with.
The Importance of Specialized Hormone Care After Cancer
But addressing them requires working with a physician who understands both oncology and hormones—who can keep you safe while actually improving your quality of life.
Personalized Cancer and Hormone Assessment
If you struggle with ongoing symptoms after cancer treatment, if your doctors have abandoned you to suffer, if you’re tired of being told there’s nothing that can be done—I invite you to schedule a Restore Pathway consultation at LifeWell MD.
Comprehensive Evaluation and Testing
We’ll review your complete cancer history. We’ll do comprehensive hormone testing. We’ll have honest conversations about what’s safe, what’s risky, what the evidence shows, and what we don’t know.
Individualized Treatment Planning
We’ll create an individualized plan that addresses your specific needs with therapies proven to work—not cookie-cutter protocols, not false promises, and never at the expense of your cancer surveillance and safety.
You beat cancer. Now let’s help you actually enjoy being alive.
Because when you walk into my office, you’re not just a cancer survivor struggling with side effects. You’re family. And family deserves better than being told to just accept suffering.
Welcome to LifeWell MD.
About Dr. Ramesh Kumar and LifeWell MD
Dr. Ramesh Kumar is a Board-Certified Medical Oncologist with over thirty years of experience treating cancer patients. After building six cancer centers across Florida’s Treasure Coast and treating more than 10,000 patients, Dr. Kumar completed advanced training in Integrative Medicine at Harvard Medical School.
He is a member of the Androgen Society and the International Society for Sexual Medicine, bringing unique expertise in both oncology and hormone optimization. Clinical guidelines recommend a multidisciplinary approach to managing menopausal symptoms in cancer survivors.
LifeWell MD provides physician-led, evidence-based survivorship care through the Restore pathway, combining rigorous oncology training with integrative medicine to address the hormonal, metabolic, and functional impairments that conventional oncology leaves untreated. Located in North Palm Beach and Port St. Lucie, Florida, serving the Palm Beach area and Florida’s Treasure Coast.
Educational Disclaimer
This article provides educational information about hormone optimization in cancer survivors based on current medical evidence and clinical experience. It does not constitute medical advice for any individual’s specific situation.
Hormone replacement therapy in cancer survivors requires careful individualized assessment considering cancer type, cancer stage, treatments received, time since treatment, current disease status, and individual risk factors. Some hormone therapies may be contraindicated in certain cancer types.
All treatment decisions should involve consultation with qualified healthcare professionals with expertise in both oncology and endocrinology. Never begin hormone therapy without comprehensive medical evaluation and ongoing monitoring. The information presented here represents Dr. Kumar’s clinical approach and interpretation of current evidence but may not reflect the views of all medical professionals or be appropriate for all patients.
Additional Info: Non-Hormonal Treatment Options for Menopausal Symptoms
For many breast cancer survivors, managing menopausal symptoms can be particularly challenging when clinicians contraindicate hormone replacement therapy (HRT) due to concerns about breast cancer recurrence or personal preference. However, effective, evidence-based non-hormonal options exist to relieve menopausal symptoms, improve quality of life, and support overall well-being for cancer survivors.
Evidence-Based Non-Hormonal Therapies
If you struggle with hot flashes, night sweats, or mood changes after breast cancer treatment, you’re not alone—and you’re not without options. Several non-hormonal medications have shown to provide real relief for menopausal symptoms in breast cancer survivors and other cancer survivors for whom hormone replacement therapy is not appropriate.
Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) rank among the most studied non-hormonal medications for treating hot flashes and vasomotor symptoms. Medications like venlafaxine, paroxetine, and citalopram can significantly reduce the frequency and severity of hot flashes, while also supporting mood and emotional well-being. These medications especially benefit breast cancer survivors who cannot use estrogen-based therapies due to the risk of breast cancer recurrence.
Gabapentin, an anticonvulsant, also decreases hot flashes, particularly when taken at night. For some women, oxybutynin—a medication more commonly used for bladder symptoms—helps manage vasomotor symptoms. These non-hormonal medications offer a safe and effective alternative to hormone replacement therapy, allowing cancer survivors to find symptom relief without increasing their risk of recurrent breast cancer.
It’s important to work closely with your healthcare provider to choose the right non-hormonal therapy for your unique situation, taking into account your cancer history, current medications, and personal preferences.
Lifestyle and Behavioral Interventions
Beyond medications, lifestyle and behavioral interventions play a powerful role in managing menopausal symptoms and enhancing quality of life for breast cancer survivors. Regular physical activity—whether it’s walking, swimming, yoga, or strength training—helps reduce the severity of hot flashes, improve sleep, and boost mood. A balanced diet rich in fruits, vegetables, and whole grains supports overall health and may help alleviate some menopausal symptoms.
Stress management techniques, such as cognitive behavioral therapy (CBT), mindfulness-based stress reduction, relaxation exercises, and advanced medical acupuncture, reduce the impact of hot flashes and improve emotional resilience. CBT, in particular, the North American Menopause Society recommends for managing menopausal symptoms in cancer survivors, as it helps reframe negative thoughts and develop practical coping strategies.
Other integrative approaches, like acupuncture, have demonstrated promise in reducing hot flashes and improving quality of life for some women. Ensuring adequate sleep, maintaining a healthy weight, and avoiding known triggers (such as spicy foods, caffeine, and alcohol) can also make a meaningful difference in managing menopausal symptoms.
For breast cancer survivors, these non-hormonal and lifestyle interventions are especially important because they provide symptom relief without increasing the risk of breast cancer recurrence. They also support long-term health by reducing the risk of cardiovascular disease, osteoporosis, and other chronic conditions that can affect cancer survivors.
The key is individualized care—working with your healthcare team to develop a plan that addresses your specific symptoms, cancer history, and personal goals. The North American Menopause Society and other professional organizations emphasize the importance of shared decision-making and evidence-based recommendations for managing menopausal symptoms in breast cancer survivors.
In summary, non-hormonal treatment options and lifestyle interventions offer a comprehensive, safe, and effective approach to managing menopausal symptoms for breast cancer survivors and other cancer survivors. By combining evidence-based non-hormonal therapies with healthy lifestyle changes, you can find real relief, improve your quality of life, and support your long-term health—all while honoring your unique cancer journey.


