[videopress qSvQsW2O]
You Beat Cancer—So Why Don’t You Feel Better?
Let me guess. You finished treatment months ago. Maybe even a year or two. The scans came back clear, and everyone congratulated you on being “cancer-free.” But here’s what nobody talks about: your body doesn’t feel like it got the memo.
The Hidden Struggles After Cancer Treatment
Persistent Fatigue and Hormonal Imbalance
You’re exhausted in a way that sleep doesn’t touch. Your hormones are all over the place.
Radiation Therapy and Tissue Damage
If you had radiation therapy—especially high-dose radiation—you might be dealing with tissue damage. Your doctors say it should heal, but it just… doesn’t.
The Role of Adjunctive Therapies
Hyperbaric Oxygen Therapy (HBOT) as a Management Tool
In these cases, adjunctive therapy, such as hyperbaric oxygen therapy (HBOT), can help manage complications from cancer treatments.
A Physician’s Perspective on Post-Cancer Care
Experience in Oncology and Integrative Medicine
I see this every single day in my practice. After thirty years treating cancer patients and building four cancer centers, I’ve watched thousands of survivors struggle with what comes after. That’s exactly why we created the Restore pathway here at LifeWell MD.
Comprehensive Care Beyond Conventional Oncology
You’ve already been through hell with chemotherapy, radiation, surgery, and other cancer treatments.
I’m Dr. Ramesh Kumar. I’m board-certified in medical oncology, and I completed my integrative medicine training at Harvard. What we do here is physician-led care that addresses what conventional oncology often leaves behind—the hormonal chaos, the metabolic dysfunction, and yes, the radiation damage that refuses to heal.
Important Disclaimer
Before we go further, here’s my standard disclaimer: Everything I’m sharing here is for education only. This isn’t medical advice for your specific situation. You need to talk with your own doctor before starting any new treatment, including HBOT. What works for one patient might not be right for another.
So When Does HBOT Actually Help Cancer Survivors?
Let me explain what HBOT actually does. You sit or lie down inside a pressurized chamber and breathe pure oxygen—and I mean truly pure, 100% medical-grade oxygen. The chamber pressurizes to levels significantly higher than normal atmospheric pressure.
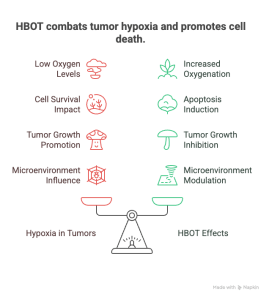
Hypoxia, a critical hallmark of solid tumors, impacts cell survival and metastasis, further complicating recovery. Moreover, the hypoxic tumor microenvironment contributes to therapy resistance and tumor progression.
Hypoxia-inducible factors (HIFs) regulate gene expression in response to low oxygen. They affect cancer cell adaptation and survival. Additionally, the tumor microenvironment, including hypoxia and reactive oxygen species, influences gene expression and cancer cell behavior. This, in turn, impacts immune modulation, inflammation, and repair mechanisms.
HBOT increases tissue oxygenation, helping to overcome tumor hypoxia. Consequently, increased oxygenation can induce apoptosis in cancer cells and may inhibit tumor growth.
Furthermore, HBOT can modulate angiogenesis and the tumor microenvironment, potentially improving therapeutic outcomes.
How HBOT Works: Pressure and Oxygen Concentration
Think about it this way. Right now, sitting at sea level, you’re at what we call 1.0 ATA—one atmosphere absolute. The air you’re breathing contains only about 21% oxygen. During real medical-grade HBOT, we take you up to 2.0 to 3.0 ATA while you breathe 100% oxygen. Your blood plasma saturates with oxygen at levels your body would never experience otherwise. We’re talking ten to twenty times more oxygen dissolved in your bloodstream.
Why Cancer Survivors Need Hyperbaric Oxygen Therapy
Now, why would a cancer survivor need this? Here’s the problem: radiation therapy kills cancer cells, but it also damages the blood vessels in the treatment area. I’ve seen it hundreds of times. As a result, the tissue becomes starved for oxygen, the blood supply diminishes, and the cells just can’t heal properly.
In normal tissues, this lack of oxygen impairs healing. Meanwhile, in tumor tissue, hypoxia can actually promote tumor progression and resistance to therapy.
You end up with this chronic, wounded state that conventional treatments can’t fix. Hypoxia, a critical hallmark of solid tumors, impacts cell survival and metastasis, further complicating recovery.
Moreover, hypoxia-inducible factors play a significant role in regulating the expression of genes involved in tumor growth and survival. This makes the hypoxic environment even more challenging to address. In tumor tissue, hypoxia stimulates the production of vascular endothelial growth factor (VEGF). VEGF promotes abnormal blood vessel formation and supports tumor angiogenesis.
HBOT has shown potential in overcoming tumor hypoxia, a key feature that drives tumor growth and therapy resistance. Additionally, hypoxia can disrupt the cell cycle and promote cell death in both normal and tumor tissues, further influencing healing and treatment outcomes.
The Healing Power of HBOT: Neovascularization and Oxygen Delivery
That’s where properly administered HBOT comes in. By flooding these tissues with oxygen under pressure, we can actually trigger new blood vessel growth. We call it neovascularization. Hyperbaric oxygenation and hyperbaric oxygen treatment have been studied in various tumor models to assess their effects on tumor angiogenesis and cellular and vascular proliferation.
The oxygen gets delivered independent of your damaged blood vessels because it’s dissolved directly in your plasma. Additionally, HBOT can promote tissue repair and reduce pain and inflammation, which may improve the quality of life for cancer patients. It has also been demonstrated to accelerate wound healing and effectively control infections related to surgical interventions in cancer patients.
Furthermore, HBOT can improve the delivery and efficacy of chemotherapy drugs by enhancing tumor perfusion. This makes it a valuable adjunct in cancer treatment. These mechanisms have been evaluated in preclinical and clinical tumor models, providing insights into how hyperbaric oxygen treatment may influence tumor microenvironment, angiogenesis, and therapeutic response.
What HBOT Is and Isn’t: Clearing Up Misconceptions
But here’s what you absolutely must understand: HBOT is not a cancer treatment. Anyone telling you it cures cancer or prevents recurrence is either ignorant or lying to you. What HBOT does—when used correctly—is heal specific complications from radiation therapy. Importantly, studies examining HBOT safety in cancer patients suggest that it does not contribute to tumor progression or worsen treatment outcomes.
Evidence indicates that HBOT does not promote tumor growth or malignant progression in patients with malignant tumors, and does not accelerate cancer progression. In fact, two systematic reviews on HBOT and cancer concluded that the use of HBOT in patients with malignancies is considered safe.
Official Approvals and Indications for HBOT in Cancer Survivors
The Undersea and Hyperbaric Medical Society, which serves as the international authority on this therapy, has approved HBOT for fifteen specific medical conditions. For cancer survivors, we focus on what they call Delayed Radiation Injuries. Moreover, the FDA agrees—they have cleared HBOT chambers as medical devices specifically for treating late radiation tissue injury.
Additionally, the FDA has approved HBOT to manage severe complications from radiation therapy and to accelerate wound healing after surgery. HBOT also acts as a radiosensitizer, improving local tumor control, especially in head and neck cancers, by enhancing radiation therapy’s effectiveness.
This process, known as tumour sensitisation, is currently being explored as a cancer treatment adjuvant and adjunctive therapy in various oncological settings. Consequently, combining HBOT with other cancer therapies may further improve outcomes.
Common Radiation Therapy Injuries Treated with HBOT
The most common problems we treat include:
Osteoradionecrosis:
It refers to bone death caused by radiation damage to blood supply. I often see this in head and neck cancer patients who received over 6,000 cGy of radiation to the jaw. The bone becomes exposed and incredibly painful. In severe cases, the jaw can fracture. The Marx Protocol prescribes thirty HBOT sessions before surgery and ten after. The success rates are remarkable for what used to be an almost untreatable condition.
Radiation cystitis and proctitis:
These affect patients who had pelvic radiation for prostate, cervical, bladder, or colorectal cancers. Symptoms include hemorrhagic bleeding, constant pain, and urgency that destroy quality of life. Radiation-induced haemorrhagic cystitis is a specific complication of radiotherapy. HBOT can help manage and heal this severe bladder injury. Recent data show about 83% of patients with radiation cystitis achieve partial or complete resolution with HBOT.
Soft tissue breakdown:
This occurs in previously irradiated areas and is another indication. These wounds won’t close despite surgical attempts. The tissue remains too damaged and oxygen-starved to heal. HBOT can improve healing by about 50%. When combined with reconstructive surgery, outcomes improve dramatically.
HBOT also treats carbon monoxide poisoning, demonstrating its broad medical applications.
Evidence-Based Use of HBOT: What It Can and Cannot Do
Let me be absolutely clear. We recommend only treatments backed by high-level evidence. I will never suggest that HBOT can cure your cancer, shrink tumors, or replace standard oncology. The science does not support that, and I won’t mislead you. Clinical analyses show cancer patients undergoing HBOT have low recurrence rates and no HBOT-related complications.
Ongoing cancer research continues to evaluate HBOT’s safety and efficacy in various oncological settings.
The Problem That’s Costing Patients Thousands
Now, I need to get direct. What I’m about to explain could save you money and heartache.
Not all HBOT is equal. Most of what wellness centers, spas, and some medical offices sell as “hyperbaric oxygen therapy” is ineffective for treating radiation injuries.
I’m not exaggerating. It literally cannot work. Yet, patients spend $15,000 to $20,000 discovering this the hard way.
The Numbers That Matter
Medical-Grade HBOT Pressure Requirements
Remember the pressure numbers I mentioned? Medical-grade HBOT requires 2.0 to 3.0 ATA with 100% oxygen. Every study showing benefit for radiation injuries used these pressures. The Marx Protocol for osteoradionecrosis specifies 2.0 to 2.4 ATA. Radiation cystitis treatment uses the same range.
Why These Pressures Matter
These pressures are not arbitrary. They achieve tissue oxygen levels needed for healing. Sustained tissue oxygen above 30 mmHg supports bone cell function and prevents bone death. Pressures of 2.0 ATA and above trigger stem cell mobilization.
The Ineffectiveness of Mild or Soft Hyperbaric Chambers
Contrast that with “mild” or “soft” hyperbaric chambers. These fabric, zippered devices operate at 1.3 ATA using regular air—still just 21% oxygen. Some use oxygen concentrators that increase oxygen to 24-26%. Even so, the physics don’t work.
Oxygen Delivery Comparison: Medical-Grade vs. Mild Chambers
Medical-grade HBOT at 2.0 ATA with 100% oxygen delivers 200% more oxygen to tissues. Mild chambers at 1.3 ATA with 21% oxygen deliver about a 6.3% increase. That’s barely above what you get walking outside.
Medical-grade HBOT delivers more than thirty times the therapeutic oxygen compared to mild chambers. Thirty times. This is not a small difference. It means mild chambers provide no therapeutic effect.
Official Guidelines on Therapeutic Hyperbaric Oxygen
The UHMS states therapeutic hyperbaric oxygen requires breathing near 100% oxygen at 1.4 ATA or greater. However, clinical practice demands at least 2.0 ATA. The European Committee of Hyperbaric Medicine specifies HBOT is valid only when oxygen partial pressure exceeds 1.5 ATA for at least 60 minutes.
Limitations of Mild Chambers for Healing Radiation Damage
Mild chambers at 1.3 ATA don’t meet the minimum threshold. They cannot be bacteriostatic. They cannot trigger stem cell mobilization. They cannot saturate tissue oxygen enough for wound healing.
For osteoradionecrosis, oxygen must penetrate deep into hypovascular, radiation-damaged bone. At 1.3 ATA with room air, this is physiologically impossible. Oxygen simply cannot reach there.
How Patients Are Being Misled
Misleading Claims by Mild Hyperbaric Oxygen Chambers
This infuriates me as a physician. Wellness centers operating mild chambers cite research done with medical-grade chambers at 2.0 to 3.0 ATA. They show impressive studies about healing radiation injuries or improving outcomes. Then they put you in a 1.3 ATA chamber and expect you to believe you get the same results.
This is not a minor oversight. It is fundamentally dishonest.
FDA Clearance and Warnings on Mild Chambers
The FDA has cleared these soft-sided chambers for exactly one thing: acute mountain sickness. That’s it. They have not cleared them for cancer-related injuries, radiation damage, osteoradionecrosis, or any of the fourteen other FDA-cleared indications for HBOT.
Moreover, the FDA has issued direct warnings about treatment centers promoting hyperbaric chambers for unapproved uses. Some mild chamber companies have faced sanctions for making fraudulent medical claims.
Safety Concerns and Risks of Mild HBOT
Even worse, the FDA, UHMS, and American Medical Association have jointly called mild HBOT “unsafe in certain settings due to dangers of fire and suffocation.” Multiple deaths have occurred from fires in these chambers. Yet, these facilities continue to operate in the largely unregulated wellness industry.
Financial and Health Consequences for Patients
When you pay $200 to $500 per session for mild HBOT claiming to heal your radiation injury, you receive no therapeutic treatment. You pay for pressurized air that delivers no more oxygen than sitting outside.
I have seen patients commit to 40-session packages—$8,000 to $20,000—before realizing nothing improves. By then, their radiation injury often worsens, requiring more extensive surgery than months earlier.
The Ethical Issue: Exploitation of Cancer Survivors
As someone who spent decades treating cancer patients, I find this exploitation of survivors unconscionable. You have endured chemotherapy, radiation, and surgery. You deserve effective treatments, not expensive placebos dressed up with borrowed credibility from real medical research.
Three Questions That Will Protect You
Before committing to any HBOT facility, ask these three questions. Their answers reveal whether you face a legitimate medical facility or a wellness center playing doctor.
Question 1: What pressure do you operate at, and what’s your oxygen concentration?
What to Expect from a Legitimate HBOT Facility
Listen carefully to their answer. You want to hear: “We operate at 2.0 ATA or higher using 100% medical-grade oxygen in FDA-cleared hard-sided chambers.”
Types of Medical-Grade HBOT Chambers
Real medical chambers come in two types. Monoplace chambers treat one patient at a time and pressurize entirely with pure oxygen. Multiplace chambers fit several patients who breathe oxygen through masks while the chamber is pressurized with compressed air. Both achieve the necessary therapeutic effect.
Red Flags: Low Pressure and Mild HBOT Claims
If they say anything about 1.5 ATA or lower, run. If they mention “soft chambers” or “mild HBOT,” you’re wasting your time. If they claim lower pressures work just as well with longer treatment times, they lie. Physiology doesn’t negotiate. You cannot make up for inadequate pressure by sitting longer.
The Truth About Mild HBOT Safety and Effectiveness
Be wary of claims that mild HBOT is “safer” or “gentler.” They mean “less effective to the point of uselessness.” Medical-grade HBOT at 2.0 to 2.4 ATA has safely treated millions over decades when protocols are followed.
Question 2: Are you UHMS-accredited?
UHMS Accreditation: The Gold Standard for Hyperbaric Facilities
You want to hear: “Yes, we’re accredited by the Undersea and Hyperbaric Medical Society. You can verify our accreditation at uhms.org/accredited-facilities.”
UHMS accreditation is the gold standard. Both the FDA and AMA recommend treatment only at UHMS-accredited facilities. This is essential, not optional.
What UHMS Accreditation Verifies
Accreditation verifies the use of FDA-cleared chambers meeting stringent safety standards. It confirms compliance with NFPA 99 Chapter 14, the mandatory fire and safety code. A qualified Medical Director supervises everything—ideally board-certified in Undersea and Hyperbaric Medicine. All staff are properly trained and certified. They follow evidence-based protocols for FDA-cleared indications.
Risks of Non-Accredited Facilities
If a facility lacks UHMS accreditation, do not proceed. No matter what they say about following guidelines or safety, no independent verification exists. They could operate with substandard equipment, unqualified staff, inadequate emergency protocols, and no real medical oversight.
Beware of False Claims
Some wellness centers claim to “follow UHMS guidelines” without accreditation. This is meaningless. Accreditation requires rigorous on-site inspection, documentation review, and ongoing compliance monitoring. It is not self-reported adherence to voluntary suggestions.
Another red flag: if they mention only having “technicians” without a board-certified hyperbaric medicine physician as Medical Director. Hyperbaric medicine involves complex physiological effects and potential emergencies—oxygen toxicity, seizures, pneumothorax complications, barotrauma. Only qualified physicians can assess contraindications, manage emergencies, and adjust protocols.
Question 3: What are your fire and safety protocols?
This question literally means life or death. They should describe strict enforcement of NFPA 99 safety rules. Specifically:
Clothing and Personal Items Restrictions
Every patient must wear 100% cotton gowns provided by the facility. No synthetic fabrics—polyester, nylon, or rayon—can ignite violently in oxygen-enriched environments. Absolutely no electronics. No cell phones, tablets, smart watches, or hearing aids unless certified for hyperbaric use. Nothing with a battery. No petroleum-based products—no makeup, lotions, oils, petroleum jelly, deodorants with aluminum, hair products, or nail polish. These create fire hazards. No jewelry or metal objects that could spark. Rigorous screening before every treatment.
Safety Equipment and Emergency Preparedness
They must have visible fire suppression systems, oxygen monitoring equipment, and emergency decompression capability. Regular staff training and emergency drills ensure readiness.
Fire Risk in Oxygen-Enriched Environments
These requirements exist because hyperbaric chambers create oxygen-enriched environments where fire spreads almost instantly. Materials normally fire-resistant become highly flammable at elevated oxygen levels. A spark from a cell phone battery or static electricity from synthetic clothing can trigger catastrophic fires.
Warning Signs to Avoid Unsafe Facilities
If a facility allows personal items in the chamber, doesn’t provide cotton gowns, seems casual about cosmetics or lotions, or downplays safety concerns—leave immediately.
Regulatory Alerts and Incidents
The FDA issued urgent safety communications in 2025 after recent fires, injuries, and deaths in HBOT facilities. Nearly all incidents occurred in facilities ignoring manufacturer instructions and safety protocols. Most involved non-accredited wellness centers using mild chambers.
The Critical Importance of Safety Protocols
People have died in hyperbaric chamber fires. Strict adherence to safety protocols distinguishes safe facilities from dangerous ones. This is non-negotiable, not paranoia, but basic medical safety.
What Real Restoration Looks Like
Medical-Grade HBOT: The Key to Effective Radiation Injury Treatment
When delivered correctly—at medical-grade pressures with pure oxygen in accredited facilities—HBOT can genuinely restore severe radiation injuries that resist conventional treatments. For the right patient with the right indication, it can be transformative.
Comprehensive Post-Cancer Recovery Beyond HBOT
However, I want you to understand that HBOT is just one tool in comprehensive post-cancer recovery.
Addressing Hormonal and Metabolic Dysfunction After Cancer
At LifeWell MD, we evaluate your hormonal function because radiation and chemotherapy often cause thyroid problems, sex hormone imbalances, adrenal insufficiency, and growth hormone deficiencies. These hormonal issues perpetuate your fatigue and rob you of quality of life. Additionally, we address radiotherapy-related complications such as osteoradionecrosis, soft tissue necrosis, and radiation cystitis, which pose serious challenges in cancer therapy.
We also assess your metabolic health, including insulin resistance, mitochondrial dysfunction, and nutrient deficiencies that prevent your cells from producing energy properly. Furthermore, we support your body’s detoxification systems, often overwhelmed by chemotherapy metabolites and radiation-induced oxidative stress.
Evidence-Based Integrative Medicine at LifeWell MD
This physician-led, evidence-based integrative medicine avoids chasing wellness trends or promoting popular social media treatments. Instead, we use therapies supported by research, with clear mechanisms of action and proven clinical outcomes. For more wellness inspiration and knowledge, explore our blog.
Ensuring Safety: Accredited Facilities and Proper Protocols
When HBOT suits your specific radiation injury, we ensure you receive it at a UHMS-accredited facility. These centers maintain proper pressures, deliver pure oxygen, and have qualified medical oversight. When other therapies like our NovoTHOR Red Light Therapy support mitochondrial function and tissue healing, we incorporate them with clear explanations of why and how they work.
Avoiding Ineffective and Costly Mild HBOT Treatments
We will never recommend a $15,000 course of mild HBOT that cannot help you. We will never suggest that HBOT cures your cancer or prevents recurrence. Moreover, we will never compromise your safety by sending you to facilities lacking proper accreditation, medical oversight, or safety protocols. These complications can prolong hospital stays and increase treatment costs. Therefore, we prioritize evidence-based, effective therapies to ensure the best outcomes for our patients.
Personalized Restore Pathway Consultations for Survivors
You deserve medicine that respects both the science of physiology and your lived experience as a cancer survivor. You deserve restoration that works—not expensive promises exploiting your hope.
If you face delayed radiation injuries, ongoing post-treatment fatigue, hormonal problems, or metabolic dysfunction after cancer, I invite you to schedule a Restore Pathway consultation at LifeWell MD. We will create an evidence-based treatment plan tailored to your specific needs. Our therapies support healing, optimize function, and restore the vitality cancer tried to take from you.
The Importance of Pressure and Purity in Oxygen Therapy and Medical Standards
When it comes to your recovery, pressure and purity matter—in oxygen therapy and in medical standards.
About Dr. Ramesh Kumar and LifeWell MD: Dr. Ramesh Kumar is a Board-Certified Medical Oncologist with advanced training in Integrative Medicine from Harvard Medical School. After treating over 10,000 cancer patients and building four cancer centers, he transitioned to integrative medicine through LifeWell MD. The center provides physician-led treatment for cancer survivors by combining evidence-based conventional medicine with scientifically validated integrative therapies. In cancer treatment, HBOT primarily acts as an adjunct therapy to enhance conventional treatments and manage side effects. Hyperbaric Oxygen Therapy (HBOT) has served for centuries to improve disorders related to hypoxia and ischemia, demonstrating its long-standing value in medical practice.
References: This article draws from current medical evidence, including the UHMS Hyperbaric Oxygen Therapy Indications Manual 15th Edition (2023), FDA guidance on HBOT devices, NFPA 99 safety standards, and peer-reviewed research on HBOT for delayed radiation injuries through 2025.


